Day #11:
My eleventh day was my first-day shadowing hospital medicine. I was initially scheduled to observe Dr. Sangani for the next five days, but she is out of town until the 29th. So, I will shadow Dr. Kaur, another hospitalist, for the next three days. Today we went floor to floor visiting sick patients and their families.
I pulled into Hillcrest's free parking tower at 7:50 AM and walked to the atrium. I took the stairs to the fourth floor and entered suite 400, across the hall from general surgery and Dr. Cha in suite 421. Dr. Kaur met me, and we walked to a back office. She introduced me to what she does as a hospitalist. Essentially, hospitalists are primary care doctors for patients recovering in the hospital. The main difference between primary care doctors (or surgeons like Dr. Hoffer and Dr. Cha) and hospitalists is that for PC doctors, the patients schedule to see their doctor, whereas a hospitalist schedules to see a patient in a rounding (room to room) fashion. Like a PC doctor, a hospitalist can diagnose illnesses, order prescriptions, and schedule imaging. They provide complete coordination over a patient from the moment they enter inpatient care to when they are discharged. Now, back to the day. She printed out a list of 13 patients we needed to cover for the day. She said that her working hours depend on how long it takes her to see the patients. We walked out of the office to our first patient on floor 3. She was an older lady–about 82–with a history of urinary tract infections (UTIs). A UTI is caused when bacteria (usually E. coli that lives naturally in the bowel) enter and infect the urinary tract. Older women are at the most risk for UTIs due to a degenerative (progressive) weakening of the internal urethral sphincter. This circular muscle allows for the voluntary flow of urine from the bladder to the urethra. The patient was put on antibiotics to fight the infection and was given IV fluid to help heal her kidneys. She was feeling better today and was scheduled to be discharged tomorrow if her vitals remained stable. The second patient we saw was a 58-year-old man. He had a history of severe diabetes, resulting in the amputation of both legs and right fingers. I understand he was initially admitted to the hospital for kidney failure. Still, throughout his stay, his overall health had deteriorated to a point where his life expectancy dropped to a few weeks. With his wife and son on the phone, Dr. Kaur recommended hospice care instead of barely keeping him alive with dialysis (a process of removing toxins from the blood when both kidneys fail). The patient accepted that he would pass soon and would like to meet with the hospice representatives tomorrow. Dr. Kaur and I left the room, and she scheduled the hospice care reps on her computer. The subsequent patients were being treated for cancer using chemotherapy (a drug that targets fast-growing cells like cancer. Unfortunately, because hair cells rapidly multiply in younger people, chemo can result in temporary baldness in that population). Both patients were scheduled to be discharged in a few days if their vitals remained stable. We also visited a patient who came in with neuropathy. Neuropathy is a collection of conditions that affects how signals travel between the brain and the central nervous system. The disorder is classified as a lower motor neuron disease, primarily affecting the appendicular system (appendages like the hands, arms, legs, and feet). Since the condition progressed a lot in the patient, he was unable to walk. Dr. Kaur scheduled him to see physical therapy (PT). The doctor ordered his discharge tomorrow to a rehab facility so that he can receive more immediate PT treatment. She finished her round around noon, so I left the clinic. Tomorrow I will be visiting many of the same patients.
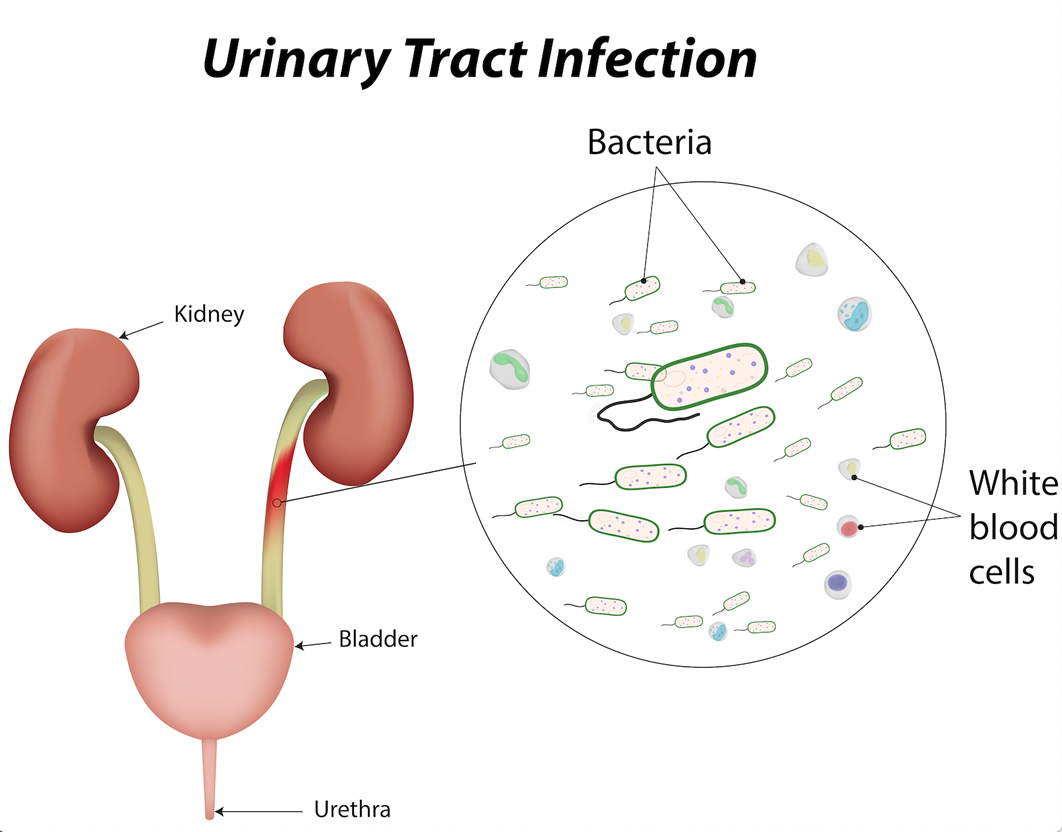
Here is an illustration of a urinary tract infection (UTI). Bacteria enter through the urethra and into the urinary tract (yellow-green). To fight the condition, the body sends white blood cells to the area, causing inflammation and pain.
Day #12:
Dr. Kaur and I rounded many of the same patients on the twelfth day.
I arrived in suite 400 at 8:00 AM this morning. I walked to the back office and met Dr. Kaur at her desk, preparing the rounds printout for the day. Today, we had fewer people to cover–around 10–so the day should be quicker. We started with the same patient from yesterday (the one with the bad UTI). Her important vitals were improving, so she was ready for discharge in the afternoon. Unfortunately, because she received a lot of IV fluid while in the ICU, much of it collected in her legs, causing them to swell up significantly. So, Dr. Kaur gave her a small dose of Lasix, a diuretic used to treat fluid retention and swelling. It was essential to limit her dose of Lasix because of her UTI. Too much would harm her healing kidneys, but too little wouldn’t allow her to urinate the excess fluid effectively. With enough time and fluids, swelling will naturally reduce, but the girth of her legs prevents her from walking. The next room was the potential hospice care patient. His wife was in the room when we entered. Unlike yesterday, the patient was much more awake and kind to the doctor and nurses. We discussed hospice again, explaining the severe drawbacks of reentering the dialysis ward. Suppose a person’s blood pressure (and blood flow) is too low. In that case, there is a possibility of undergoing myocardial infarction (heart attack) while in dialysis because the heart has to work harder to pump less blood, leading to excess straining and potential arrest. We will check back in with the patient and his family tomorrow to hear their decision. While Dr. Kaur was checking his breathing with her stethoscope, out of nowhere, the patient looked into her eyes and kept thanking her. It was a wholesome moment for everyone in the room. The next patient we saw was the cancer patient from yesterday who was undergoing chemotherapy. He was drained and lethargic from the chemo and had short episodes of intense coughing whenever he took deep breaths. Dr. Kaur gave him some cough medicine, and the nurse refilled one of his IV tubes with an antibiotic. If he continued in the same direction, he would be discharged tomorrow. Her next patient was new: a 95-year-old woman who was admitted to the hospital for heart issues. The patient explained that she lived independently and would experience chest pain a few times a month. We will check in with her tomorrow once all of her vitals return, and Dr. Kaur can make a better prognosis on her heart condition. Then we revisited the other patient undergoing chemo for blood cancer. She was healing quite rapidly and would also be discharged tomorrow. One of the last patients we saw was a patient with neuropathy. His discharge to rehab was in a few hours, so Dr. Kaur wanted to say a few parting words. Apparently, his mother, who was in her late 90s, requested that she drive him to the facility; pretty ironic, considering the situation. The doctor and the patient shook hands while he thanked her for her care over the past few days. Then Dr. Kaur and I returned to suite 400, where I collected my bag and left Hillcrest. Tomorrow, we will see a few new patients and revisit some previous ones.
Here is a dialysis machine. First, blood is drawn from an arterial (artery) opening in the patient's body and fed through a pump in the machine. Then the blood is taken to a dialyzer (far right) filter to remove toxins unable to be removed by the kidneys. From there, the blood is pumped into an air trap which purges the air from the blood. Air bubbles in the blood can cause an air embolism when circulated to the brain, heart, or lungs, resulting in heart attacks, strokes, or respiratory (lung) failures. So, removing any air is necessary to keep the patient healthy. Once the air is removed from the blood, anti-clotting medication is pumped into the tube, and the blood reenters the body through a separate venous (vein) opening.
:max_bytes(150000):strip_icc()/RENAL_DIALYSIS-56a275235f9b58b7d0cac1e2.jpg)
Comments
Post a Comment